Surgery for Obesity
Bariatric Surgery or Surgery for morbid Obesity What patients/candidates should know
What is Obesity? What are the health hazards because of obesity?
Obesity means having excess body fat in relation to ones height and weight. Obesity generally is determined by calculating body mass index (BMI), which is calculated by the weight in kilograms divided by height in meters squared.
| BMI | Status 1 |
|---|---|
| 18.5 – 24.9 | Normal |
| 25 – 29.9 | Over weight |
| 30 – 34.9 | Obese |
| 35 – 39.9 | Severe Obesity |
| > 40 | Morbid Obesity |
| > 50 | Super morbid Obesity |
* Among Asian Indians, the recommended BMI for obesity surgery is >32.5 with co=morbid illnesses and >37.5 in Obese individuals. (Consensus Statement for diagnosis and treatment of Obesity, JAPI, Vol.57, February 2009. www.japi.org)
1. National Institutes of Health and National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res 1998;6(suppl 2):1S-209S.
Severe obesity damages the body by its mechanical, metabolic and physiological adverse effects on normal bodily function. These "co-morbidities" affect nearly every organ in the body in some way, and produce serious secondary illnesses, which may also be life-threatening. The following are the excess risk of associated illnesses related to obesity.
| Co-Morbidity | Percentage of more risk |
|---|---|
| Diabetes | 20-40% |
| Hypertension | 25-55% |
| Hyperlipidemia | 35-53% |
| Cardiac disease | 15-25% |
| Respiratory disease | 10-20% |
| sleep apnea | 20-30% |
| Arthritis | 20-30% |
| Depression | 70-90% |
| Stress Incontinence | 40-50% |
| Menstrual irregularity | 15-25% |
With BMI > 30 there is 55% increase in mortality, 70% increase in coronary artery disease, 75% increase in stroke and 40% increase in diabetes. So, morbidly obese males between 25 and 35 have 12x the chance of dying as normal weight men. A morbidly obese adult has a 33% less chance of living to age 65 as that of a normal weight person. That is the reason why surgery for obesity has great relevance in treating the excess weight and cures/ improves most of these medical conditions along with the surgery.
What is Bariatric surgery? How is it different from liposuction?
Bariatric surgery involves surgical methods to restrict or to reduce absorption of food from stomach and intestine. This is not a cosmetic surgery. This procedure results in overall reduction in bodyweight and helps to improve associated medical disorders of excess bodyweight. Liposuction is a cosmetic surgery wherein part of body fat is removed using high power suction, which usually does not produce any sustained weight loss.
Who should undergo this procedure?
As a first line of treatment diet and exercises should be tried. Patients who had a trial of diet, regular exercise and probably drugs and failed to have a sustained weight loss must think about this surgery. Among Asian Indians, the recommended BMI for obesity surgery is >32.5 with co=morbid illnesses and >37.5 in Obese individuals. (Consensus Statement for diagnosis and treatment of Obesity, JAPI, Vol.57, February 2009. www.japi.org)
How effective is weight-loss surgery? What are the benefits and is the effect long term?
These procedures help in reducing 50-85% excess body weight. The amount of weight loss varies depending on the type of procedure chosen (usually done by the doctor). Along with weight loss most of the medical co-morbidities improve which in turn improves patients self esteem and confidence. Some of the important benefits are
- Diabetes mellitus Type II in these patients improve and a vast majority of them become completely normal blood sugar levels normal after surgery.
- Hypertension & high cholesterol improves significantly. These effects along with good amount of weight loss reduce risk for heart disease significantly.
- There is good relief for sleep problems, apnoea and acid reflux symptoms.
- As the body weight comes down body pain and joint arthritis improves very well.
- Overall improvement in the sense of well being and self esteem.
The effect of these procedures is long term in terms of weight loss and improvement of co-morbidities, if the patient adheres to the follow up advice of the doctor
Type of Bariatric surgery:
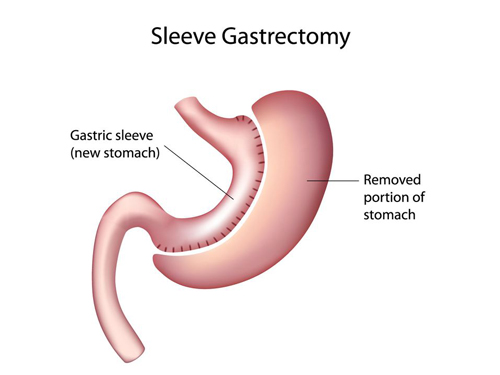
Laparoscopic Sleeve Gastrectomy:
Laparoscopic Sleeve Gastrectomy is a restrictive operation which changes size of the stomach. A small gastric reservoir is created that reduces the stomach size to 60-150 ml.
The operation involves the removal of the upper rounded part of your stomach called the fundus. The fundus is one of the parts of the stomach that produces ghrelin, the hormone that controls your appetite. Gastric sleeve surgery, also known as the sleeve gastrectomy, has become a popular choice for patients seeking excellent weight loss in a straightforward procedure that doesn’t require the maintenance drugs or long term medications.
Laparoscopic Sleeve Gastrectomy has the benefits below:
- May reduce hunger.
- The hunger inducing hormone ghrelin is reduced by removing a portion of the stomach largely responsible for its production.
- Reduction of hunger occurs in most patients but not all.
- Shorter operating time compared to gastric bypass.
- Does not re-route intestines.
- No dumping syndrome.
- Generally doesn’t produce any long term nutritional deficiencies.
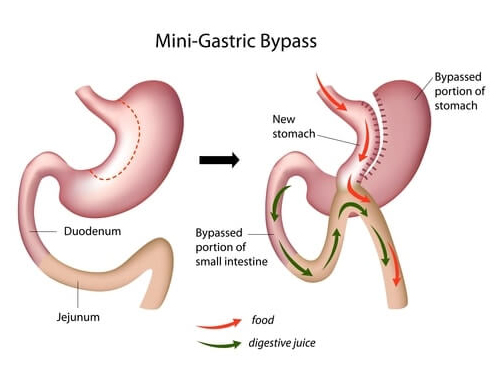
Laparoscopic Gastric Bypass procedures:
Mini gastric bypass surgery (MGBP) makes the stomach smaller and reroutes the intestines. As a result, patients:
- Feel full sooner while eating
- Absorb fewer calories and minerals
- Lose up to 3/4 of their excess weight within 2 years
- Have significant health improvement
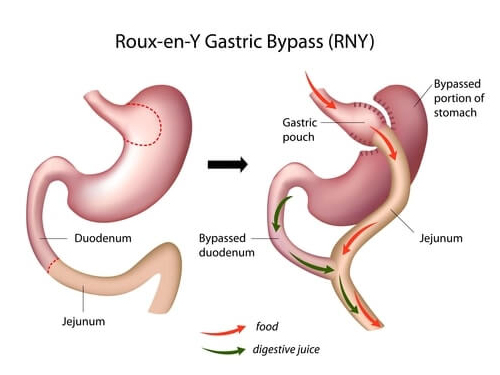
Compared to the more widely performed Roux-en-Y gastric bypass procedure (“gastric bypass”), mini gastric bypass studies show similar weight loss and health improvement, a lower risk of complications, and fewer and less severe side effects. Unlike gastric bypass, MGBP is also reversible, and MGBP costs less for self-pay patients.
Gastric bypass surgery refers to a surgical procedure in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass (GBP) procedures. Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.